I believe that technology has a central role to play in improving how public services, including healthcare, are delivered. However, like many who work with the public sector, I have often struggled with finding the best way to use technology to solve problems quickly. Rapidly implementing digital innovation in the NHS, for example, is a challenge. There are good reasons for this; the relentlessly iterative ‘fail-fast’ mentality so popular in the private sector seems inappropriate when you are spending public money. A more purposeful approach towards technology innovation is usually adopted, but this is slower than typical agile software delivery.
But then the Covid-19 pandemic happened. Suddenly, there were complex, dynamic, fast-moving, technical challenges that required complex, dynamic, fast-moving, technical responses.
In my role supporting the delivery of the NHS Test and Trace programme, everything I knew to be true about the speed of public service technology change was challenged. In responding to a global pandemic, I saw how the NHS, and public sector organisations more broadly, could be capable of fast-paced, agile implementation. In this article, I’ll share with you some of things I learned from this experience and how it has changed the way I will approach public sector projects going forward.
Building the supply chain for mass testing
In late 2020, as England prepared for its first Covid winter, the Department of Health and Social Care (DHSC), at the time the body responsible for NHS Test and Trace (NHSTT), needed to scale up the supply chain of Lateral Flow Device (LFD) test kits. Between November 2020 and January 2021, BJSS and several other suppliers supported DHSC and NHSTT in building the supply chain technology capability to ensure a coherent, coordinated approach to Covid-19 LFD test supply. The ambition was to build an enduring supply chain technology platform, one capable of responding not just to the current pandemic, but to the next one, too.
In my role as Lead Architect, I provided technical expertise and solutions to help DHSC meet the challenges in the most timely and technically effective way, as well as organising the teams already working in this area to achieve a coordinated approach. This included defining the technical strategy and growing the technology delivery capability through services and people to make sure it happened.
Getting The Right Test To The Right Location In The Right Volumes
The NHS Test and Trace programme was stood up from scratch at the beginning of the Covid-19 pandemic and tasked with an almost impossible challenge: react and respond to the pandemic on a day-to-day, hour-to-hour basis, across a variety of clinical and patient-facing factors and touchpoints.
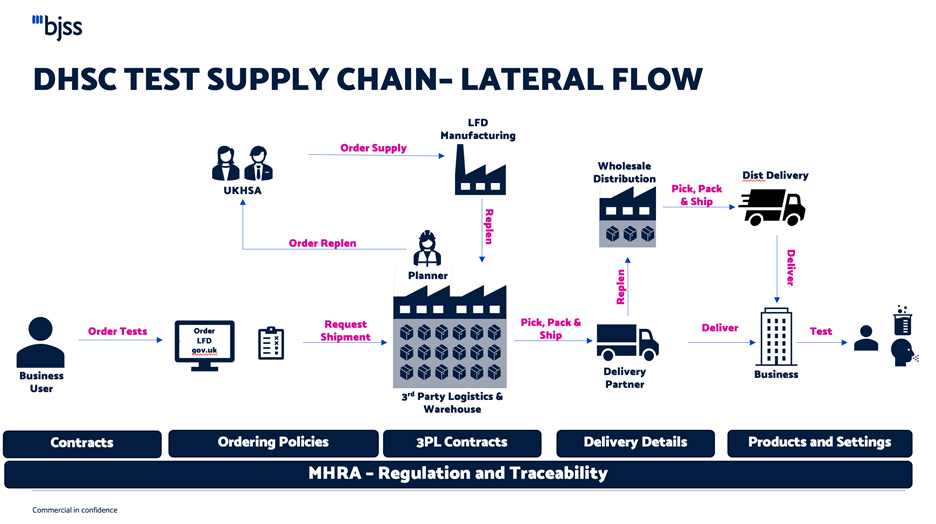
Across the extensive ecosystem of activity, one of the many challenges was ensuring the supply of LFD tests to the UK population. This included all clinical settings, such as hospitals, GP practices and care homes, as well as schools, universities, and other access points, such as pharmacies.
If you’re in England and reading this, chances are you’ve received a pack of LFDs in the post. But to get the tests from the factory floor to your front door (not to mention all the other endpoints I mentioned above), an entire supply chain had to be established from scratch. Together with the other technology partners working on this project, we had to consider every step of the process and answer questions like:
- What products do we have in which location?
- How many locations do we need to deliver to?
- What size of orders go into which delivery flow?
- Which suppliers can fulfil a lorry order (for example, for school testing)?
- Which suppliers can fulfil orders through your letterbox?
Ultimately, running the test supply chain is about getting the right testing supplies to the right organisation in the right volume. The need was for technology to facilitate that process with the flexibility to support the various suppliers, test types, and geographic locations required – all while reacting to demand for tests at a national level. And, of course, because LFDs are medical devices, the technology would need to comply with medical regulations set out by the Medicine and Healthcare products Regulatory Agency (MHRA), but also be adaptable to changes in policies and priorities as the situation evolved. No easy feat!
From Concept To Go-Live In Five Weeks
They say Rome wasn’t built in a day. To that I’d add, neither was Amazon. In fact, any company known for ‘nailing’ supply chain technology has developed its technologies over many years, or, at the very least, months. We had even less than that to create our supply chain solution. And, given the significance of the work, we were already on borrowed time.
So, what did we do? First, we rapidly mapped the value chain to understand the enabling set of capabilities supporting the supply chain business. Through capturing the high-level business architecture, we were able to identify the key constraints and what needed to be addressed first. Once we developed this value chain, we assessed the technology capability against the business needs.
Working with the DHSC and its partners, we were able to define and agree a technology strategy. We were then able to rapidly define the big chunks of work in the form of a Portfolio Epic. It took a lot of effort, but we worked together to establish a governance and operating model across teams, address the technology requirements, and deliver a technical solution to the test supply chain challenge at pace.
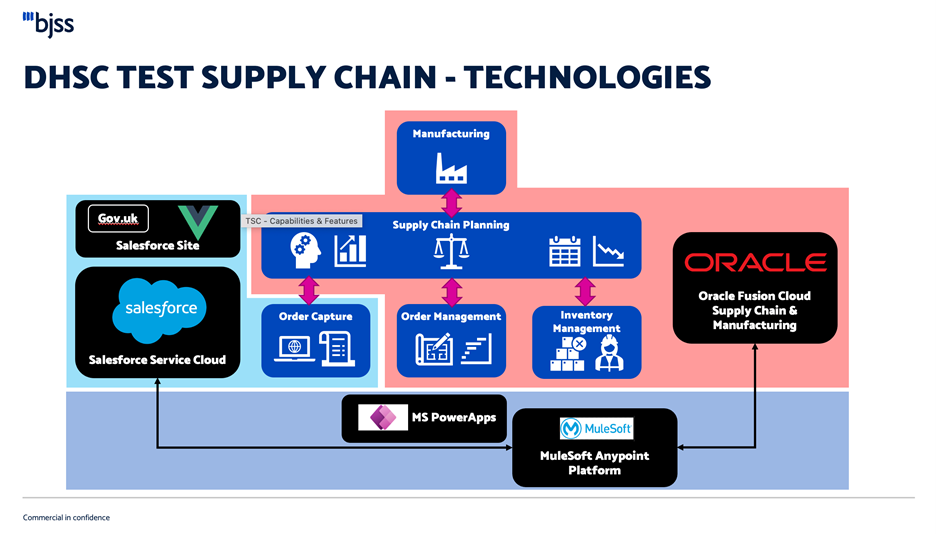
We built a low-code integration between SalesForce and Oracle Inventory Management and Order Management. The integration was built using MuleSoft, which allowed a closed loop between orders captured in SalesForce, flowing to inventory and order management, and the 3PL for delivery to the customer. We then extended the implementation of Order Management and supply chain planning to cover lateral flow tests.
From conception to go live, this low-code piece was done within five weeks, enabling a working solution that could then be developed incrementally, both to improve functionality and to be responsive to the changing needs of those responding to the pandemic.
Shifting My Technical Paradigm
As technologists working with the public sector, our role is to be innovative but also responsible. We must consider the most efficient and sustainable way to deliver long-term solutions that meet the public need. It’s why, prior to working on this project, I would shudder if anyone used the term ‘throwaway technology’ regarding a solution for the NHS. It would be unconscionable to spend taxpayer money on rapidly developing technology that you know won’t be used in the long term, even if valuable learnings came from the process. I thought that, in many ways, there were limits to how agile one could be when delivering software solutions in this space.
My work with the NHS Test and Trace programme has shifted my thinking on this somewhat. When faced with the contradictory requirements of developing an enduring solution and a tactical solution, we were given the permission of necessity and realised we could deliver some phenomenal solutions that strike the balance of both.
My main takeaway is this: that it’s not necessarily about failing fast or being cautious but finding the balance between the two. The way we work at BJSS, taking an agile approach but with strong project governance, gives us the flexibility to make good, but fast, decisions. The BJSS model of collaborative working also means we can ensure the right people are doing the right work at the right time; we aren’t precious about having all the answers, so long as we can bring the necessary people together to innovate and deliver.
Where Do We Go From Here?
Demand for testing will continue into 2022. The UK Heath Security Agency (UKHSA), the agency now responsible for the NHS Test and Trace programme, will continue to develop its supply chain technology for mass testing, improving and iterating to meet the ever-evolving demand.
BJSS continues to support the UKHSA and the rest of the NHS in implementing innovative digital solutions. We are also keen to capture learnings and explore how they can be applied to other clients. To this end, in November 2021, I presented our experiences working on the NHS Test and Trace supply chain to our Health & Social Care Community of Practice. We had a lively discussion about what we learned and how to bring this to our work at BJSS. And I, for one, believe that we can implement dynamic, fast-moving, agile solutions that are sustainable and meet the needs of the public.
Published
April 29, 2024Reading time
5 minutesRelated posts

.svg)



